Program designed to combat rising drug prices
WOONSOCKET, R.I. — CVS Health has revealed a new, comprehensive program designed to combat rising prescription drug prices and help patients save money on their medications.
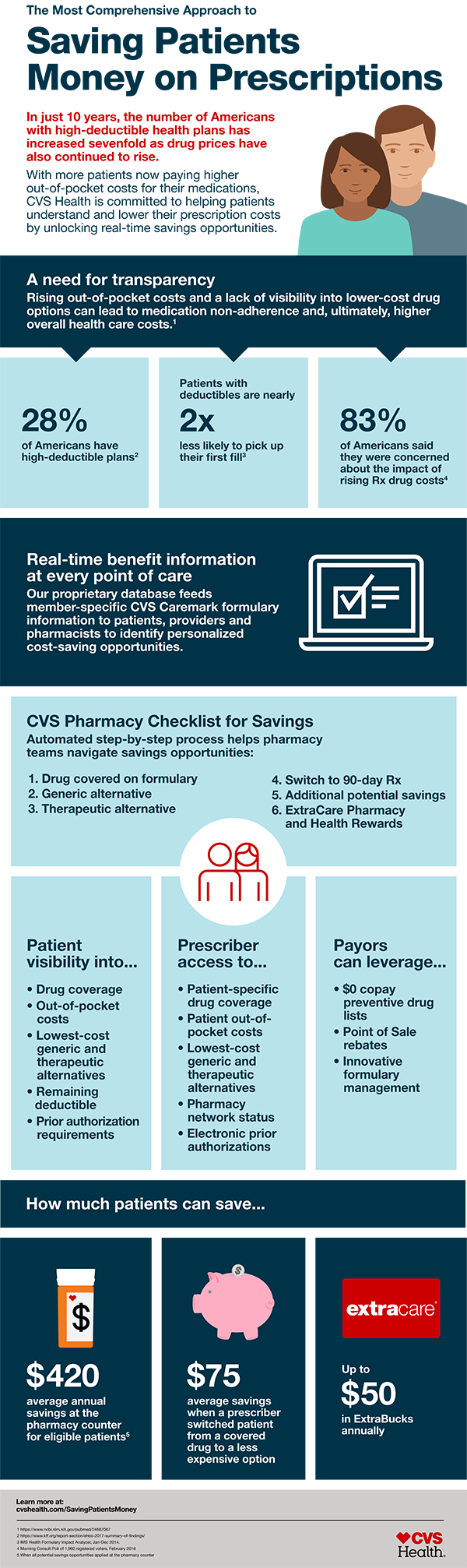
The new initiatives are being launched against a background of ongoing increases in manufacturers’ list prices for drugs and a growing percentage of Americans who have high-deductible health plans. A recent Morning Consult poll commissioned by CVS indicates that 83% of respondents are personally concerned about the impact of rising prescription drug prices.
With more and more Americans joining high-deductible health plans, more patients are incurring higher out-of-pocket costs for their medications. These patients are twice as likely not to fill their prescriptions when confronted with the cost.
At the heart of the program is a new initiative, the CVS Pharmacy Rx Savings Finder, which for the first time enables the company’s retail pharmacists to evaluate quickly and seamlessly, at the pharmacy counter, opportunities to save on individual scripts. The new tool leverages technology and CVS enterprise data to give pharmacists access to real-time information for each patient and enable them to review the patient’s prescription regimen and insurance plan information to determine the best way to reduce their out-of-pocket costs.
“Today’s consumers are faced with higher prescription drug prices than ever before, and many of them are now paying for a larger share of their prescription drug costs out of their own pockets at the pharmacy counter due to growth in high-deductible health plans,” says Thomas Moriarty, chief policy and external affairs officer of CVS Health. “Until now, patients haven’t had the appropriate tools available to them to help them manage these costs. To address this, CVS Health is giving expanded tools to patients, prescribers and pharmacists so they can evaluate prescription drug coverage in real time and identify lower-cost alternatives.
“We are committed to finding the right drug at the lowest possible cost for patients to ensure they are able to access and stay on the medications they need.”
According to a company spokeswoman, the catalyst for the creation of Rx Savings Finder was the daily feedback CVS receives from consumers about the complexity of trying to find a solution to drug pricing on their own. Patients, she points out, have no single resource for guidance, instead having to check with their insurance company or their doctor, or even go online to search for manufacturer coupons and other information.
“Our direct experience is that patients who are confronted with high out-of-pocket costs at the pharmacy counter are less likely to pick up their prescriptions and are less likely to be adherent to their prescribed therapy,” remarks Kevin Hourican, executive vice president of retail pharmacy at CVS Pharmacy. “Armed with the information available through our Rx Savings Finder, our more than 30,000 CVS pharmacists can play an important role by helping patients save money on their medications, providing advice on how and when to take them, and ultimately helping them achieve better health outcomes.
“We are beginning this process with our CVS Caremark PBM members and expect to roll it out more broadly through the year.”
Specifically, the Rx Savings Finder allows the pharmacist to see if the prescribed drug is on the patient’s formulary and if it is the lowest-cost option available. It also informs the pharmacist whether there are lower-priced options — such as a generic or a therapeutic alternative with equivalent efficacy — that are covered under the patient’s pharmacy benefit. It also indicates whether the patient might be able to save money by filling a 90-day script instead of a 30-day prescription.
If neither a generic nor another lower-cost alternative is available, the program indicates other potential savings options for eligible or uninsured patients, where allowed by applicable laws and regulations. Scripts submitted for reimbursement to Medicare, Medicaid or other federal and state programs, however, are not eligible.
Using the Rx Savings Finder, the pharmacist can also help patients enroll in CVS’s ExtraCare loyalty program and sign them up for Pharmacy and Health Rewards, which enable patients to receive $5 in ExtraBucks for every 10 prescriptions filled, up to a total of $50 annually.
The new initiatives are not limited to the pharmacy. CVS recently launched a real-time benefits program that gives health care providers and CVS Caremark members greater drug price transparency. At the point of prescribing, providers can see the member-specific cost for a selected drug, based on the member’s coverage, as well as up to five lowest-cost, clinically appropriate therapeutic alternatives, based on the patient’s formulary.
CVS Caremark members can access the same information on the CVS Caremark app and member portal. According to the company, early results from this program show that prescribers who accessed the real-time benefits information through their electronic health records system switched their patient’s drug from a non-covered drug to a drug on the formulary 85% of the time.
In addition, when the patient’s drug was covered, prescribers used the benefits information to switch the patient to a lower-cost alternative 30% of the time. In those cases, the average difference in the cost of the script was approximately $75.
CVS is also making available a variety of solutions available to its PBM clients to help further drive down drug costs for them and the patients they support. For example, the company’s Point of Sale rebate allows negotiated rebates on branded drugs to be passed on directly to patients when they fill a prescription. That program was introduced in 2013 and now nearly 10 million members are eligible to benefit from it.
Last year, the company points out, in spite of an increase of nearly 10% in branded drug list prices, CVS Caremark was able to limit drug price growth for its members to a minimal 0.2%. Consequently, 42% of CVS Caremark commercial clients spent less on their pharmacy benefit plan last year than in 2016. The PBM further helped its members reduce monthly out-of-pocket costs and improve adherence by patients to the highest level in seven years in such key categories as diabetes, hypertension and hyperlipidemia.
“We have been working hard to keep prescription medications affordable for patients,” says Dr. Troy Brennan, executive vice president and chief medical officer at CVS Health. “In fact, in 2017 nearly 90% of our PBM plan members spent less than $300 out of pocket for their prescription medicines. While this signals progress for those patients, that cost is not insignificant.
“That is why we are committed to doing even more across our enterprise to help patients find and access the lowest-cost drug at the pharmacy, which ultimately will help improve clinical outcomes and remove higher downstream medical costs from the system.”




You must be logged in to post a comment Login